Medical Device Software and Digital Health: Revolutionizing Healthcare
The healthcare industry has undergone a significant transformation in recent years, driven by advancements in technology and data analytics. Medical device software and digital health have emerged as key players in this revolution, transforming the way healthcare is delivered, managed, and experienced.
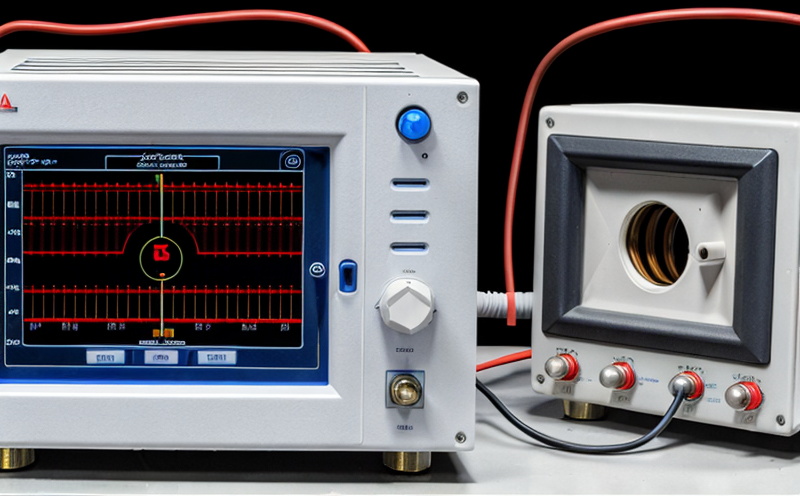
At its core, medical device software refers to the programming and coding that enable medical devices to function. These devices range from simple insulin pumps to complex imaging machines like MRI and CT scanners. The software embedded within these devices can be categorized into three primary types: control software, application software, and middleware.
Control software is responsible for controlling the basic functions of a device, such as power management, communication protocols, and data transmission. Application software, on the other hand, provides the user interface and functionality that clinicians and patients interact with daily. Middleware acts as an intermediary between different systems, facilitating data exchange and integration between various medical devices.
Digital health encompasses a broader scope than medical device software alone. It involves the application of digital technologies to improve healthcare outcomes, enhance patient engagement, and streamline clinical workflows. Digital health includes mobile health (mHealth), telehealth, personal health records (PHRs), and electronic health records (EHRs). These innovations have created new avenues for delivering care, promoting preventive measures, and tracking treatment efficacy.
The Rise of Medical Device Software: Key Benefits
Improved Patient Outcomes: Advanced medical device software enables the creation of more precise and personalized treatment plans. For instance, insulin pumps with integrated glucose monitoring systems allow patients to adjust their medication levels in real-time, preventing hypoglycemia episodes and improving overall glycemic control.
Increased Efficiency: Automation through medical device software reduces manual errors, streamlines clinical workflows, and minimizes healthcare-associated infections. Medical devices can now be remotely monitored, reducing the need for on-site visits and facilitating timely intervention when issues arise.
Enhanced Data Collection and Analysis: The integration of medical device software with EHRs and other digital health tools facilitates comprehensive data collection and analysis. This information is essential for clinicians to make informed decisions, optimize treatment strategies, and identify areas for improvement.
Digital Health: Transforming Healthcare through Technology
Telehealth and Remote Monitoring: Telehealth platforms enable patients to consult with healthcare professionals remotely, reducing the need for in-person visits and improving access to care, especially for underserved populations. Remote monitoring technologies allow clinicians to track vital signs and treatment progress from afar, promoting early intervention and reducing hospital readmissions.
Mobile Health (mHealth) and Personal Health Records (PHRs): mHealth applications empower patients with personalized health insights, enabling them to take a more proactive role in their care. PHRs provide secure storage for patient medical history, medication lists, and allergy information, facilitating seamless communication between healthcare providers and patients.
Electronic Health Records (EHRs) and Interoperability: EHRs standardize clinical data exchange across different healthcare settings, ensuring that critical patient information is accessible whenever needed. Interoperability solutions enable seamless integration of medical devices with EHRs and other digital health tools, eliminating data silos and promoting holistic care.
QA: Additional Insights into Medical Device Software and Digital Health
Q1: What are the primary challenges facing medical device software developers?
A1: Developers must balance competing priorities, such as regulatory compliance, user experience, and system performance. They must also ensure seamless integration with existing EHRs and other digital health tools.
Q2: Can you elaborate on the differences between control software, application software, and middleware in medical devices?
A2: Control software focuses on basic device functions, while application software provides the user interface and advanced functionality. Middleware acts as an intermediary, facilitating data exchange between different systems.
Q3: What are some potential risks associated with relying too heavily on digital health technologies?
A3: Over-reliance on digital tools can lead to decreased human interaction and empathy, potentially eroding patient relationships and trust in the healthcare system. Additionally, digital solutions may not account for individual needs or contextual factors that influence treatment outcomes.
Q4: How do regulatory agencies ensure the safety and effectiveness of medical device software?
A4: Regulatory bodies like the FDA and EU MDR establish guidelines and standards for medical device development, ensuring that software meets strict quality control and clinical validation requirements. These regulations evolve as new technologies emerge and healthcare needs change.
Q5: What are some emerging trends in digital health that may shape the future of healthcare delivery?
A5: Artificial intelligence (AI) is increasingly being integrated into digital health platforms to analyze large datasets, predict patient outcomes, and personalize treatment plans. Additionally, blockchain technology has been explored for secure data storage and transmission in healthcare.
Q6: Can you discuss the role of cloud computing in medical device software development and deployment?
A6: Cloud-based infrastructure enables developers to create scalable, flexible systems that accommodate changing user needs and regulatory requirements. It also facilitates remote monitoring and real-time analytics, improving overall system performance and patient care.
Q7: What are some common misconceptions about medical device software and digital health?
A7: Many clinicians and patients believe that digital solutions eliminate the need for human interaction or physical examination. However, these technologies complement traditional care methods, augmenting patient relationships and enhancing treatment outcomes when used judiciously.
By embracing the potential of medical device software and digital health, we can create a more connected, data-driven healthcare ecosystem that prioritizes patient-centered care and promotes seamless communication between clinicians, patients, and caregivers. As technology continues to evolve, it is essential for healthcare stakeholders to collaborate and address emerging challenges, ensuring that these innovations remain accessible, safe, and effective for all.